- Facet joint Radiofrequency Thermocoagulation (RFT) Treatment
- Radiofrequency Thermocoagulation Dorsal root ganglion (DRG) radiofrequency thermocoagulation (RFT)
- Discitis Procedure
- Sacroiliac Joint Radiofrequency Treatment (Simplicity)
- In-Disc Ozone Therapy
- Nucleoplasty
- Transforaminal Injection (Pinpoint)
- Facet joint block
- Epidural Injection
Neuropathic Pain and Neuralgia
- Home
- Neuropathic Pain and Neuralgia
Contents
Toggle- Creating an individualised treatment plan
- The role of different specialities (physiotherapist, orthopaedist, psychologist, neurosurgeon)
- Pain treatment during pregnancy
- Treatment of chronic pain in the elderly
- Pain management in children
- Stress management
- Healthy eating
- Ergonomic living arrangements
- Exercise and mobility
- Facet joint Radiofrequency Thermocoagulation (RFT) Treatment
- Radiofrequency Thermocoagulation Dorsal root ganglion (DRG) radiofrequency thermocoagulation (RFT)
- Discitis Procedure
- Sacroiliac Joint Radiofrequency Treatment (Simplicity)
- In-Disc Ozone Therapy
- Nucleoplasty
- Transforaminal Injection (Pinpoint)
- Facet joint block
- Epidural Injection
- Cancer pain
- Permanent Epidural / Spinal Port Application
- Vascular Port (Permanent Vascular Access)
- Trigeminal Nerve RFT
- Blockade of Ganglion Stellatum
- Lumbar Sympathetic Ablation
- Facet joint Radiofrequency Thermocoagulation (RFT) Treatment
- Radiofrequency Thermocoagulation Dorsal root ganglion (DRG) radiofrequency thermocoagulation (RFT)
- Hernia Burning (IDET)
- Discitis Procedure
- Sacroiliac Joint Radiofrequency Treatment (Simplicity)
- Permanent Epidural / Spinal Port - Pump System
- In-Disc Ozone Therapy
- Nucleoplasty
- Peripheral Nerve Block
- Transforaminal Injection (Pinpoint)
- Facet joint block
- Epidural Injection
- Intra-articular Fluid Treatment
- Dorsal root ganglion (DRG) radiofrequency thermocoagulation (RFT)
- Spinal cord stimulation (pain pacemaker)
- Ergonomic living arrangements
- Spinal cord stimulation (pain pacemaker)
- Nucleoplasty
- Radiofrequency ablation
- Herbal solutions
- Dry needle treatment
- Anti-ageing treatments
- Ozone therapy
- Cupping therapy - Cupping
- Mesotherapy
- Prolotherapy
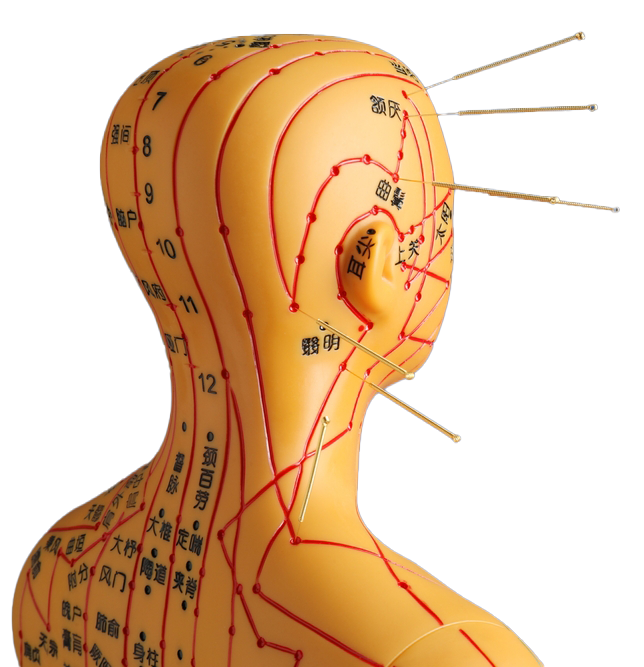
- Acupuncture
- Stem Cell Therapy
- Nerve blockages
- Corticosteroid injections
- Massage and relaxation techniques
- Manual therapy
- Electrotherapy
- Neuropathic pain medications
- Anti-inflammatory drugs
- Muscle relaxants
- Painkillers (paracetamol, ibuprofen, etc.)
Neuropathic pain is a type of pain, often described as "burning", "electric shock" or "tingling", which is caused by damage or disorder in the nervous system (central or peripheral). It is often not adequately controlled by conventional painkillers (e.g. nonsteroidal anti-inflammatory drugs or simple painkillers). Many different causes and mechanisms can underlie this type of pain; neuropathic pain can develop in a wide range of conditions ranging from diabetes to traumatic nerve injuries, infections and rheumatic diseases.
Neuralgia is a type of neuropathic pain that is felt in the area of distribution of a specific nerve or group of nerves and is of sudden onset, often in attacks and severe. A well-known example is "trigeminal neuralgia", in which the trigeminal nerve (the large nerve responsible for facial sensation) is affected. Even with simple stimuli such as chewing, touching or talking, this condition can cause sharp pain in certain parts of the face, like an "electric shock".
Below you will find comprehensive information on neuropathic pain and neuralgia, symptoms, diagnostic methods and treatment approaches.
1. General Characteristics of Neuropathic Pain
- Description
- It is a form of pain that occurs when nerve tissue is damaged or dysfunction develops.
- Unlike somatic or visceral pain, it can also be felt without the need for "real" tissue damage.
- Symptoms and Pain Character
- Burning, stinging, tingling, pins and needles similar unexplained sensations.
- Like an electric shock, sharp, like a lightning strike pain attacks.
- Hypersensitivity to cold or hot contact (allodynia), painful perception of stimuli that should not normally cause pain (e.g. light touch).
- Pain, which sometimes increases at night, can disrupt sleep and reduce quality of life.
- Common Causes
- Diabetic Neuropathy: One of the long-term complications of diabetes; It is seen as burning and tingling, especially in the feet and legs.
- Trigeminal Neuralgia: Very severe and sudden attacks of pain radiating to the face (described in more detail below).
- Postherpetic Neuralgia (Pain after Shingles): Chronic, burning pain in the area of the rash after herpes zoster (shingles) infection, which persists despite healing.
- Peripheral Nerve Injuries: Trauma, surgical incisions or impingement (tarsal tunnel, carpal tunnel, etc.).
- Spinal Cord Injuries: Neuropathic pain may occur in areas below certain segments.
- Multiple Sclerosis (MS), Parkinson's, Spinal cord tumour such as neurological diseases.
- Chemotherapy Drugs or nerve damage by other toxic substances.
- Diagnosis
- Detailed history of the patient (how the pain started, its character, localisation, spread, accompanying symptoms).
- Neurological examination (light touch, needle test, hot-cold discrimination, reflexes).
- Blood tests (diabetes, B12 deficiency, thyroid function, etc.).
- EMG (electromyography) and Nerve Conduction Studies: Detection of conduction disorders in nerves.
- Imaging methods (MRI, CT, etc.) in suspicion of underlying tumour, compression, structural lesion.
2. Neuralgias: Special Cases
2.1 Trigeminal Neuralgia
- Description: The fifth cranial nerve (trigeminal nerve) arising from the brain stem provides facial sensation. As a result of irritation of various branches of this nerve, electric shock-like pain attacks occur in the face (usually in the chin, cheek and forehead areas).
- Symptoms:
- Attacks of pain that are very short-lived but extremely severe.
- It can be triggered even by simple stimuli such as talking, chewing, brushing teeth, shaving, wind blowing.
- Attacks can last from a few seconds to a few minutes and may recur throughout the day.
- Causes:
- Compression of the nerve by a vessel or other structure (microvascular compression).
- Multiple sclerosis or brain stem/cranial nerve lesions.
- Sometimes no definite underlying cause can be found (idiopathic).
- Treatment:
- Medication Therapy: Antiepileptic drugs such as carbamazepine, oxcarbazepine are the first step. Other neuropathic pain medications such as gabapentin, pregabalin may also be used.
- Interventional Methods: Radiofrequency thermocoagulation, glycerol injection, balloon compression (pain relief by destroying the pain fibres of the nerve).
- Surgery: Microvascular decompression (separation of the compressing vessel from the nerve) or gamma knife radiosurgery.
2.2 Postherpetic Neuralgia (Pain after Shingles)
- Description: Pain, often severe and burning, which may persist even after the herpes zoster (reactivation of the chickenpox virus) rash has healed.
- Symptoms:
- Burning, pins and needles, sensitivity to touch in the skin area of the rash.
- It can be in the form of sharp pain in attacks or constant aching.
- Risk Factors:
- Especially advanced age, weakened immune system.
- Although the pain does not start immediately after the shingles infection, it can occur within weeks or months.
- Treatment:
- Antiviral drugs (early initiation during shingles reduces the risk of postherpetic neuralgia).
- Neuropathic pain medications (gabapentin, pregabalin, TCA antidepressants).
- Pain patches (containing lidocaine or capsaicin) can provide localised relief.
2.3 Occipital Neuralgia
- Description: Sharp pain in the back of the head and nape of the neck due to irritation or compression of the occipital nerves (nerves that innervate the back of the head and the back of the ear).
- Causes: Tension in the neck muscles, trauma, degenerative spine diseases can be confused with tension-type headache.
- Treatment: Local injections, neuropathic painkillers, physiotherapy (cervical spine stabilisation), rarely surgery.
2.4 Glossopharyngeal Neuralgia
- Description: Irritation of the 9th cranial nerve (glossopharyngeal nerve). It manifests as severe, attack-like pain radiating to the back of the tongue, tonsils, throat, ear and sometimes under the jaw.
- Symptoms: Stabbing pain in the throat/ear that can be triggered by swallowing, talking, coughing or yawning.
- Treatment: Antiepileptics (carbamazepine, gabapentin etc.), nerve blocks, rarely surgery.
3. Treatment of Neuropathic Pain
- Medication Therapy
- Antidepressants: Tricyclic antidepressants (amitriptyline, nortriptyline), SNRIs (duloxetine, venlafaxine). Especially effective in chronic conditions such as diabetic neuropathy or fibromyalgia.
- Antiepileptics: Drugs that reduce the hyperexcitability of nerve cells such as carbamazepine, gabapentin, pregabalin, oxcarbazepine, lamotrigine.
- Topical Agents: Lidocaine patches, capsaicin creams. It may be useful in superficial nerve pain.
- Opioids: If the pain is severe and does not respond to other treatments, it can be used under the supervision of a doctor. It should be approached with caution due to the risks of long-term addiction and side effects.
- Interventional Methods
- Nerve Blocks: Injection of drugs or substances that have a temporary or permanent effect on the nerve (e.g. glycerol injection for the trigeminal nerve).
- Epidural / Intrathecal Drug Applications: Direct administration of painkillers by inserting a catheter around the spinal cord.
- Spinal Cord Stimulation: Electrodes placed on the spinal cord membrane are used to block the transmission of pain signals. It is used in chronic and resistant pain.
- Surgical Methods: Microvascular decompression or radiofrequency ablation techniques, especially in specific conditions such as trigeminal neuralgia.
- Physiotherapy and Rehabilitation
- Reducing muscle tension with light exercises, stretching and strengthening movements, relaxation techniques.
- Contributing to nerve healing by increasing circulation.
- Applications such as TENS (Transcutaneous Electrical Nerve Stimulation) can also reduce pain perception in some patients.
- Psychological Support and Approach
- Chronic neuropathic pain may increase the risk of depression and anxiety.
- Methods such as cognitive behavioural therapy, relaxation exercises and stress management relieve the emotional burden of pain.
- Lifestyle Adjustments
- Diabetes Control: Monitoring blood sugar at regular intervals, eating a balanced diet and exercising to prevent and slow down diabetic neuropathy.
- Eliminating Vitamin Deficiencies: B12 deficiency in particular can cause nerve damage.
- Reducing / Quitting Smoking and Alcohol Consumption: May increase the risk of nerve damage and vascular problems.
4. Important Tips for Neuralgia and Neuropathic Pain
- Early Diagnosis
- Correct classification of the type of pain is critical for determining the treatment.
- If there are burning or stinging complaints that do not go away with ordinary painkillers, a neurology or algology specialist should be consulted immediately.
- Personalisation of Treatment
- Each patient has a different pain threshold, underlying cause and comorbidities.
- The dosage, combination and additional treatment methods should be individually adjusted.
- Long Term Follow-up
- Some neuropathic pain may not disappear completely; it may require chronic management.
- Side effects, efficacy level and quality of life of the patient should be evaluated at regular intervals.
- Psychosocial Support
- Patients may have difficulty performing daily activities and experience social isolation due to intense pain attacks.
- Family, friends and professional support (physiotherapist, psychologist) are very valuable in this process.
- Co-operation of Different Medical Branches
- Depending on the cause of the pain, it may be necessary to work together with branches such as neurosurgery, physiotherapy, endocrinology (diabetes), oncology (cancer-induced neuropathy) and rheumatology.
5. When to seek emergency medical help?
- Sudden and Severe Pain If "new" has developed, especially if attacks similar to electric shocks have become frequent, especially in the face, head or any part of the body.
- Gait, Balance or Movement Disorders begins (there may be progressive damage to the nervous system).
- Numbness, weakness in the arms or legs if it increases significantly.
- If Pain Cannot Be Controlled Despite Medication or if the pain intensifies.
- Serious Psychological Problems (depression, suicidal thoughts).
In such cases, it is important to have a specialist physician's assessment and, if necessary, emergency intervention without delay.
Summary
Neuropathic pain and neuralgias are types of pain that arise from damage or dysfunction in the nervous system and are usually perceived as burning, sharp, electric shock. Although the mechanism and triggers of pain may differ in specific examples such as trigeminal neuralgia, postherpetic neuralgia, diabetic neuropathy, the principles of treatment are generally similar.
Various drug combinations, especially antiepileptic and antidepressants, nerve blocks, surgical methods and physical/psychological support approaches are applied in treatment. The most effective results are achieved with a multidisciplinary approach to the cause of the pain and personalised treatment planning. Controlling the pain greatly improves the patient's quality of life and allows them to continue their daily life activities in a healthier way.
Our treatments
- Home
- Neuropathic Pain and Neuralgia