- Facet joint Radiofrequency Thermocoagulation (RFT) Treatment
- Radiofrequency Thermocoagulation Dorsal root ganglion (DRG) radiofrequency thermocoagulation (RFT)
- Discitis Procedure
- Sacroiliac Joint Radiofrequency Treatment (Simplicity)
- In-Disc Ozone Therapy
- Nucleoplasty
- Transforaminal Injection (Pinpoint)
- Facet joint block
- Epidural Injection
Lower Abdominal Pain
- Home
- Lower Abdominal Pain
Contents
Toggle- Creating an individualised treatment plan
- The role of different specialities (physiotherapist, orthopaedist, psychologist, neurosurgeon)
- Pain treatment during pregnancy
- Treatment of chronic pain in the elderly
- Pain management in children
- Stress management
- Healthy eating
- Ergonomic living arrangements
- Exercise and mobility
- Facet joint Radiofrequency Thermocoagulation (RFT) Treatment
- Radiofrequency Thermocoagulation Dorsal root ganglion (DRG) radiofrequency thermocoagulation (RFT)
- Discitis Procedure
- Sacroiliac Joint Radiofrequency Treatment (Simplicity)
- In-Disc Ozone Therapy
- Nucleoplasty
- Transforaminal Injection (Pinpoint)
- Facet joint block
- Epidural Injection
- Cancer pain
- Permanent Epidural / Spinal Port Application
- Vascular Port (Permanent Vascular Access)
- Trigeminal Nerve RFT
- Blockade of Ganglion Stellatum
- Lumbar Sympathetic Ablation
- Facet joint Radiofrequency Thermocoagulation (RFT) Treatment
- Radiofrequency Thermocoagulation Dorsal root ganglion (DRG) radiofrequency thermocoagulation (RFT)
- Hernia Burning (IDET)
- Discitis Procedure
- Sacroiliac Joint Radiofrequency Treatment (Simplicity)
- Permanent Epidural / Spinal Port - Pump System
- In-Disc Ozone Therapy
- Nucleoplasty
- Peripheral Nerve Block
- Transforaminal Injection (Pinpoint)
- Facet joint block
- Epidural Injection
- Intra-articular Fluid Treatment
- Dorsal root ganglion (DRG) radiofrequency thermocoagulation (RFT)
- Spinal cord stimulation (pain pacemaker)
- Ergonomic living arrangements
- Spinal cord stimulation (pain pacemaker)
- Nucleoplasty
- Radiofrequency ablation
- Herbal solutions
- Dry needle treatment
- Anti-ageing treatments
- Ozone therapy
- Cupping therapy - Cupping
- Mesotherapy
- Prolotherapy
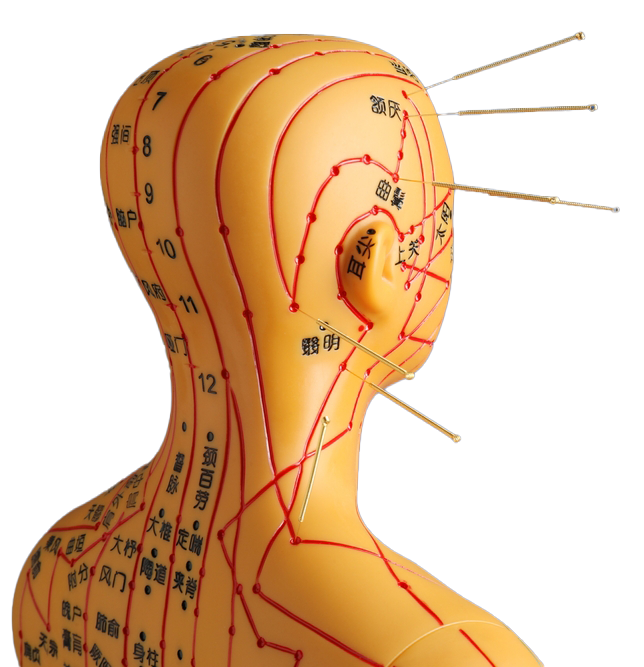
- Acupuncture
- Stem Cell Therapy
- Nerve blockages
- Corticosteroid injections
- Massage and relaxation techniques
- Manual therapy
- Electrotherapy
- Neuropathic pain medications
- Anti-inflammatory drugs
- Muscle relaxants
- Painkillers (paracetamol, ibuprofen, etc.)
Pain in the lower abdomen can be caused by many different reasons, regardless of men and women. While some of them may be simple and temporary, in some cases they may be a harbinger of serious health problems. Lower abdominal (pelvic) pain can be caused by problems with the digestive system, urinary tract, reproductive organs or musculoskeletal system. Below you will find a more comprehensive overview of common causes of lower abdominal pain, diagnostic methods and precautions that can be taken.
1. Common Causes of Lower Abdominal Pain
1.1 Digestive System Causes
- Constipation, Gas Pains and Digestive Disorders
- Bloating, cramp-like pain in the lower abdomen, partial relief after passing gas or needing the toilet.
- Factors such as excessive fibre-free diet, insufficient fluid intake, inactivity can trigger.
- Irritable Bowel Syndrome (IBS)
- A chronic intestinal disorder with attacks of abdominal pain, bloating, constipation or diarrhoea.
- Sensitivity to stress may increase the severity of symptoms.
- Inflammatory Bowel Diseases (Crohn, Ulcerative Colitis)
- Symptoms such as persistent or intermittent lower abdominal pain, diarrhoea, bloody stools, weight loss, fatigue.
- Abdominal pain, especially in the form of cramps, occurs in recurrent attacks.
- Intestinal Infections (Gastroenteritis)
- Infections of the stomach and intestines caused by bacteria, viruses or parasites.
- It may progress with symptoms such as abdominal pain, diarrhoea, nausea, vomiting and fever.
- Appendicitis
- Severe and increasing pain in the lower right side of the abdomen, nausea, vomiting, sometimes accompanied by mild fever.
- Usually the pain starts around the umbilicus and localises to the right lower quadrant.
- Diverticulitis
- Inflammation of small pockets (diverticula) at the end of the large intestine, especially in the elderly or those on a fibre-free diet.
- There may be pain in the left lower quadrant, fever, constipation or diarrhoea.
1.2 Reproductive Organ Causes (Female)
- Menstrual Pain (Dysmenorrhoea)
- Cramp-like pain in the lower abdomen and lower back during or close to menstruation.
- Sometimes accompanied by nausea, headache and weakness.
- Endometriosis
- A chronic condition in which the inner tissue of the uterus (endometrium) settles outside the uterus and forms inflammation and adhesions.
- Symptoms such as intense menstrual pain, painful sexual intercourse, chronic pelvic pain.
- Ovarian Cysts
- Occasional pain, bloating or a feeling of fullness in the lower abdomen.
- When some cysts burst or twist (cyst torsion), sudden and severe pain can occur (emergency).
- Pelvic Inflammatory Disease (PID)
- Infections involving the uterus, ovaries or tubes.
- Symptoms such as persistent pain in the lower abdomen, fever, discharge, pain during intercourse or urination.
- Ectopic Pregnancy (Ectopic Pregnancy)
- The fertilised egg implants in the tubes or other parts of the body instead of the uterus.
- Lower abdominal pain, vaginal bleeding, dizziness, low blood pressure (in emergencies such as ruptured tubes) may occur.
1.3 Reproductive Organ Causes (Male)
- Prostatitis (Prostate Inflammation)
- Pain in the lower abdomen or groin, burning when urinating, frequent urination, sometimes fever and chills.
- It can be divided into acute or chronic prostatitis; symptoms vary according to severity.
- Testicular Problems (Orchitis, Epididymitis, Testicular Torsion)
- There may be additional findings such as pain radiating to the groin and lower abdomen, swelling, redness, fever.
- Testicular torsion (rotation of the testicle) requires urgent intervention and can cause severe pain in the groin and lower abdomen.
- Inguinal Hernia
- Swelling in the groin area, pain with heavy lifting or straining.
- If the swelling is compressed (strangulated hernia), the pain intensifies and may require emergency surgery.
1.4 Urinary Tract Causes
- Urinary Tract Infection (UTI)
- Frequent urge to urinate, burning or pain when urinating, sometimes pain in the lower abdomen or groin area.
- If fever and weakness are added, pyelonephritis (kidney inflammation) may be considered.
- Kidney and Ureteral Stones
- When stones descend from the kidney into the ureter (urinary canal), a severe pain called "renal colic" may occur.
- Pain may radiate from the waist to the groin, nausea, vomiting and blood in the urine may be observed.
1.5 Musculoskeletal and Other Causes
- Muscle Strain and Hernias (Abdominal Wall Hernia)
- Injury to the abdominal muscles as a result of excessive exercise, heavy lifting or sports injuries.
- Localised pain that increases with touch or movement.
- Stress and Psychological Factors
- Especially in diseases such as IBS (Irritable Bowel Syndrome), stress can increase the severity of pain.
- Other Rare Causes
- Spinal problems reflected in the lower abdomen (herniated disc, etc.).
- Intra-abdominal tumours or masses.
- More serious and rare conditions such as vascular occlusions (e.g. mesenteric vascular occlusion).
2. Additional symptoms that may accompany lower abdominal pain
- Fever, Chills: It may be an infection or inflammatory condition.
- Nausea, Vomiting: Appendicitis, intestinal infections, kidney stone crises etc. can be seen in tables.
- Diarrhoea or Constipation: Digestive system problems (IBS, intestinal infection, diverticulitis, etc.).
- Vaginal discharge or bleeding (for women): Reproductive organ problems (PID, ectopic pregnancy, menstrual cycle disorders, etc.).
- Burning, Frequent Urination, Blood in Urine: Urinary tract infections or stones.
- Swelling in the groin: Possible hernia.
- Pain during sexual intercourse (for women): Pelvic diseases such as endometriosis, PID.
These symptoms provide important clues about the cause of the pain and help the physician in the diagnosis.
3. Diagnostic Methods
- Medical History and Physical Examination
- Questioning the location, type, intensity, triggering factors and other symptoms associated with pain.
- Abdominal examination, listening to bowel sounds, palpation (e.g. McBurney's point for suspected appendicitis).
- Laboratory Tests
- Blood Tests: Complete blood count (elevated WBC may indicate inflammation), CRP, Sedimentation etc.
- Urinalysis: To evaluate conditions such as urinary tract infection, kidney stones.
- Faecal Tests: Infectious agent or blood occult test.
- Imaging Methods
- Ultrasound: It is often used to examine the female reproductive organs (ovarian cysts, fibroids), prostate, kidney and bladder.
- Computed Tomography (CT) or Magnetic Resonance (MR): In more complex cases or suspected appendicitis, diverticulitis, intestinal obstruction, tumour.
- Endoscopic Investigations: Colonoscopy or gastroscopy can be performed to detect diseases of the digestive system.
- Gynaecological Examination
- Gynaecological ultrasound, pelvic examination, cervical swab tests (suspicion of PID, ectopic pregnancy, etc.).
- Special Tests
- Beta-hCG: If pregnancy or ectopic pregnancy is suspected in women.
- Hormone Tests: Endometriosis or other reproductive diseases.
4. Treatment Methods
The treatment of lower abdominal pain varies greatly depending on the cause:
- Medical (Drug) Treatments
- Antibiotics: Bacterial infections (urinary tract infection, PID) or diverticulitis.
- Anti-inflammatory and Painkillers: Symptomatic treatment of conditions such as appendicitis, costochondritis, menstrual pain or endometriosis pain.
- Muscle Relaxants/Antispasmodics: IBS or spasmodic intestinal pain.
- Birth Control Pills or Hormone Treatments: Endometriosis, extremely painful menstrual cycle.
- Prostate Medicines: Pain associated with prostatitis or enlarged prostate.
- Surgical Interventions
- Appendicitis Surgery (Appendectomy): Definite or strongly suspected appendicitis.
- Hernia Repair: Inguinal hernia or abdominal wall hernia.
- Ovarian Cyst Removal, Ectopic Pregnancy Operation gynaecological surgeries, etc.
- Bowel Surgery: Obstruction, perforation, advanced diverticulitis or Crohn's complications.
- Lifestyle Changes and Supportive Therapies
- Dietary Modification: High-fibre foods, plenty of water consumption, foods that regulate the intestinal flora (probiotics) are especially useful in IBS and constipation.
- Regular Exercise: Regulates digestion, improves circulation, reduces stress.
- Stress Management: Meditation, yoga, therapy approaches in stress-triggered conditions such as IBS.
- Hot Application: A hot compress on the lower abdomen can reduce muscle spasm, especially in menstrual cramps or muscle-related pain.
- Physical Therapy / Pelvic Floor Exercises
- Exercises to strengthen and relax the lower abdominal and pelvic muscles can help with chronic pelvic pain.
5. Simple precautions that can be taken in daily life
- Balanced Nutrition
- Eating enough fibre, limiting fast food and excessive fatty foods.
- Drink plenty of fluids (on average 1.5-2 litres of water per day).
- Regular Physical Activity
- Moderate exercise such as walking, swimming and cycling regulates bowel movements.
- Getting rid of excess weight can reduce intra-abdominal pressure.
- Organising Toilet Habits
- Not to hold faeces for a long time, not to postpone the need for toilet.
- Do not ignore constipation or diarrhoea for a long time.
- Personal Hygiene and Protection
- Especially for women, changing pads and tampons frequently during menstruation, keeping the genital area clean and dry.
- Safe sexual intercourse practices against sexually transmitted diseases.
- Avoiding / Managing Stress
- Stress can trigger many digestive and pelvic problems. Relaxation techniques and, if necessary, psychological support are important.
- Periodic Health Checks
- Women should have regular gynaecological examinations (ovarian cysts, fibroids, infections, etc. can be detected early).
- Men should not neglect prostate health check-ups (especially those aged 50 and over).
6. When to consult a doctor?
Lower abdominal pain may be mild and temporary, or it may be a sign of serious conditions. In the following cases, medical help should be sought immediately:
- The pain is severe and persistent, lasting for more than a few hours but not relieved.
- Fire, nausea and vomiting, diarrhoea or constipation is accompanied by severe symptoms such as.
- marked abdominal stiffness, tension and hypersensitivity to touch if it occurred.
- Bloody faeces, bloody vomiting or blood in the urine if any.
- Pallor, cold sweat, extreme weakness, feeling faint if there are signs of a general disturbance of the general condition, such as
- Ectopic pregnancy suspicion, abnormal vaginal bleeding or very severe non-menstrual pain.
- Testicular torsion or severe pain that requires "emergency intervention", such as strangulated inguinal hernia.
Summary
Since lower abdominal pain can be caused by quite different reasons, it is not possible to talk about a single treatment approach. The important thing is to perform a detailed examination and necessary examinations to correctly identify the source of the pain. Common gynaecological causes in women (ovarian cyst, endometriosis, pelvic inflammation, etc.), prostatitis, testicular diseases or inguinal hernia in men should be examined in detail. Infections of the digestive system and urinary tract are also the main causes of lower abdominal pain.
The treatment may include medication, surgical interventions, lifestyle modifications and, if necessary, physiotherapy or psychological support. If the pain is mild, it can be monitored primarily with simple precautions and rest; if it is severe and prolonged, it is of great importance to consult a healthcare professional to determine the cause and start appropriate treatment.
Our treatments
- Home
- Lower Abdominal Pain